CLINICAL
Hypertensive disorders in ART pregnancies (Project Leader: Dr. Anna Blázquez)
Pre-eclampsia is a disorder with potential severe neonatal and maternal complications that is increased in pregnancies achieved by ART. We know that pregnancies achieved by oocyte donation or by sperm donation are at a high risk of pre-eclampsia, and some recent studies also claim that after frozen embryo transfer the prevalence of this syndrome increases. Our objective is to improve our understanding of its pathogenesis to be able to develop better prophylactic measures and treatments interventions in populations at risk. Our studies focus on the different theories of the etiology of pre-eclampsia. In one study we studied characteristics and reproductive outcomes of double-gamete donation pregnancies (Blázquez et al 2016). Another ongoing study compares oocyte donation gestations obtained by fresh embryo transfer vs. frozen embryo transfer, with the aim of understanding the role of the embryo and the endometrium in the trigger of pre-eclampsia. A third study focuses on the relationship between pre-eclampsia and maternal cardiovascular disease.
Optimization of training in ART procedures (Project Leader: Dr. Amelia Rodríguez)
Several procedures within assisted reproduction are operator-dependent and as such can be subject to be standardized, taught/learned and monitored during both training and clinical practice. Optimizing the training in the technical procedures involved in ART is crucial to reach high-quality standards in medical care.
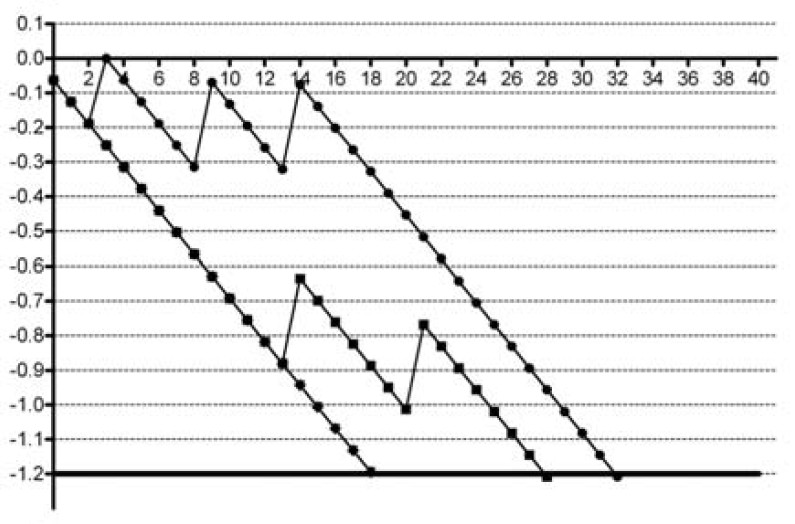
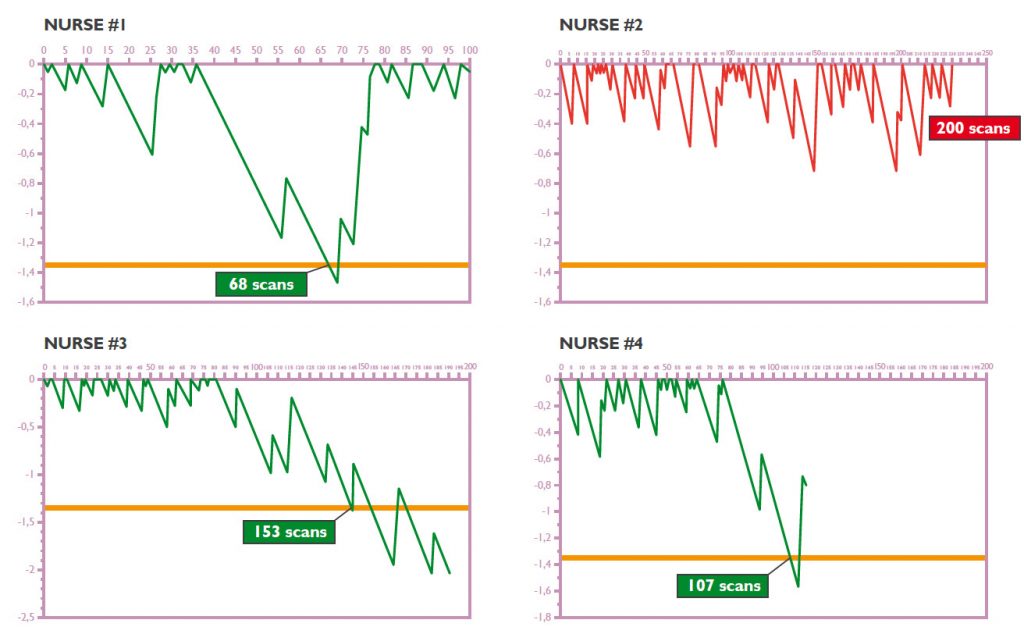
During the last several years, we have carried out a series of studies to personalize and assess the learning of several IVF steps. The method we use, CUSUM (Cumulative Summation), and its derived Cumulative Summation test for Learning Curve (LC-CUSUM), can help in quantifying the number of procedures needed to become competent in a technique.
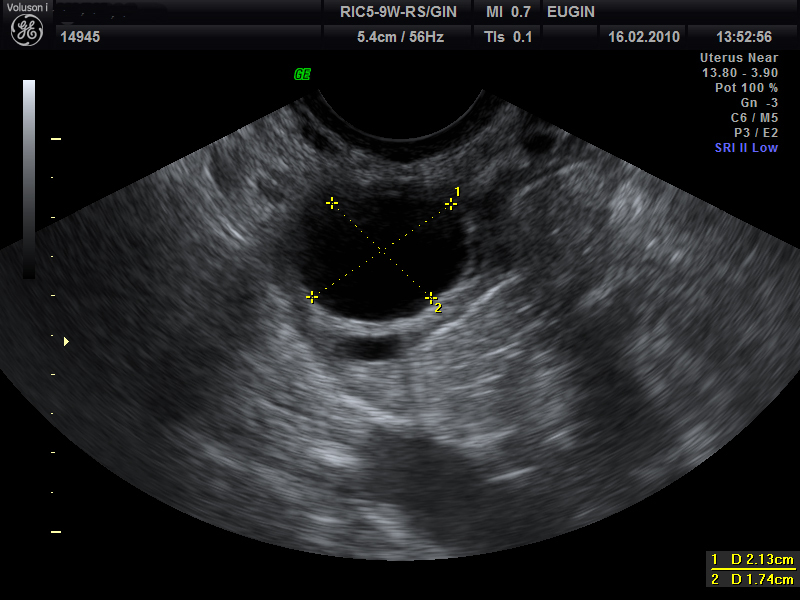
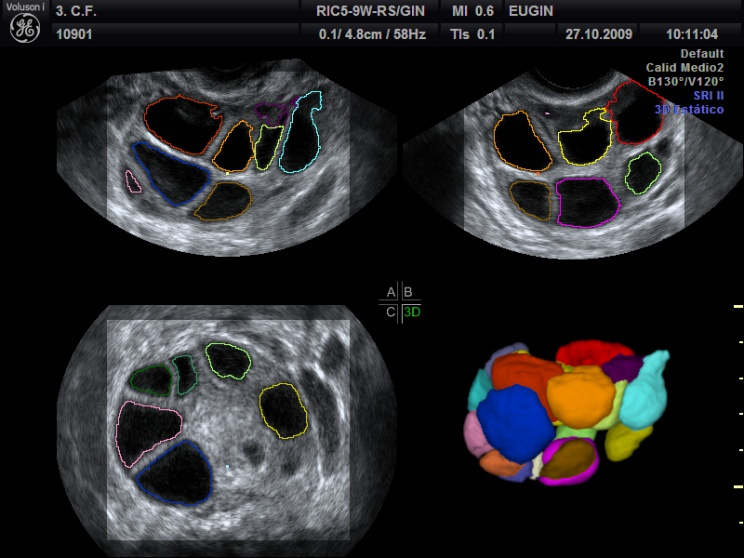
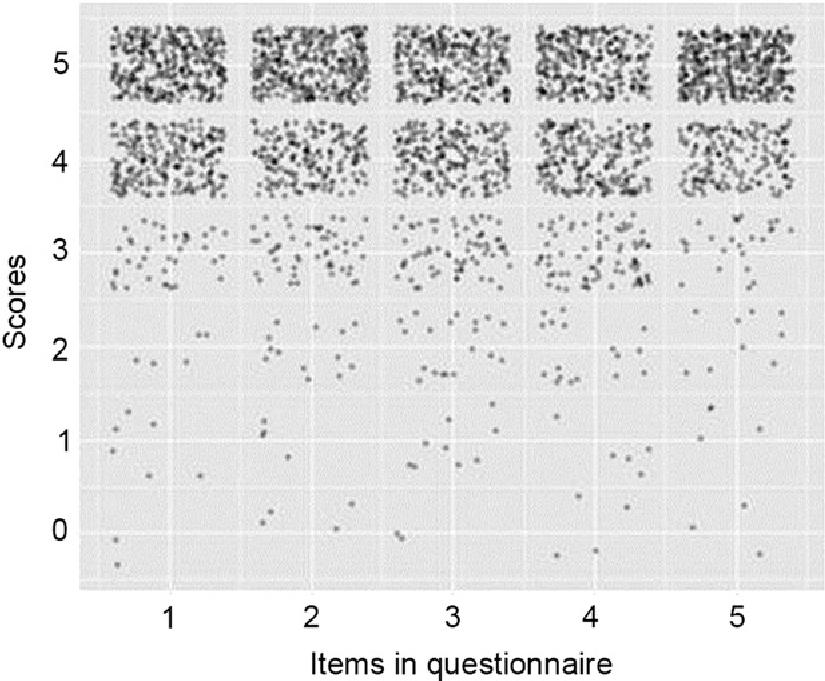
Up to date, we have applied the LC-CUSUM to the learning of 3D follicular monitoring during controlled ovarian stimulation (Rodríguez 2014), embryo transfer (López 2014), and also in laboratory techniques such as ICSI (Durban 2016). We have found, for instance that the number of procedures to reach competence in 3D follicular monitoring oscillates between 19 and 38 in physicians with previous experience in 2D monitoring, amount that can be absolutely assumed by a medium size fertility center (Figure 3). The specific training on 3D follicular monitoring in nurses without previous experience in follicular monitoring and follow-up with the LC-CUSUM tool showed that most nurses (6/8) acquired competence within the first 200 procedures (Figure 4).
Moreover, this research has allowed us to include of paramedical personnel (nurses and laboratory technicians) in technical procedures usually performed by physicians or embryologists.
PARAMEDICAL
Fertility knowledge and awareness (Project Leader: Dr. Désirée García)
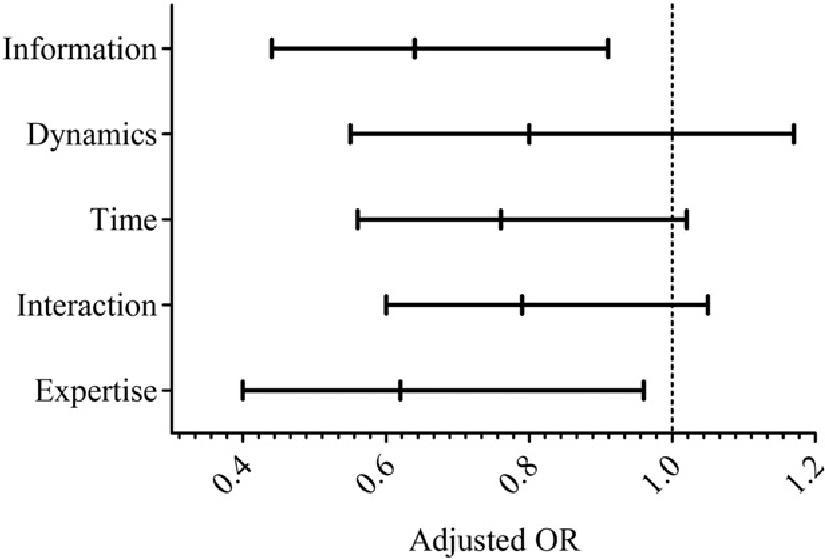
Patient-centered care is mainly based in information, communication, respect, and emotional support, aspects of care that should be provided by all the personnel of an ART center. In this research line we are interested in the continued education and formation of our physicians, not only in technical procedures, but also in empathic skills. The training proposed aimed to provide personnel of tools to improve information provision and communication with patients. We demonstrated a significant improvement in patient satisfaction after the training (Figure 1, García 2013). Currently, we have adapted this training to other personnel of the center (nurses, embryologists) and we continue to closely follow the demand of our patients in terms of emotional support.
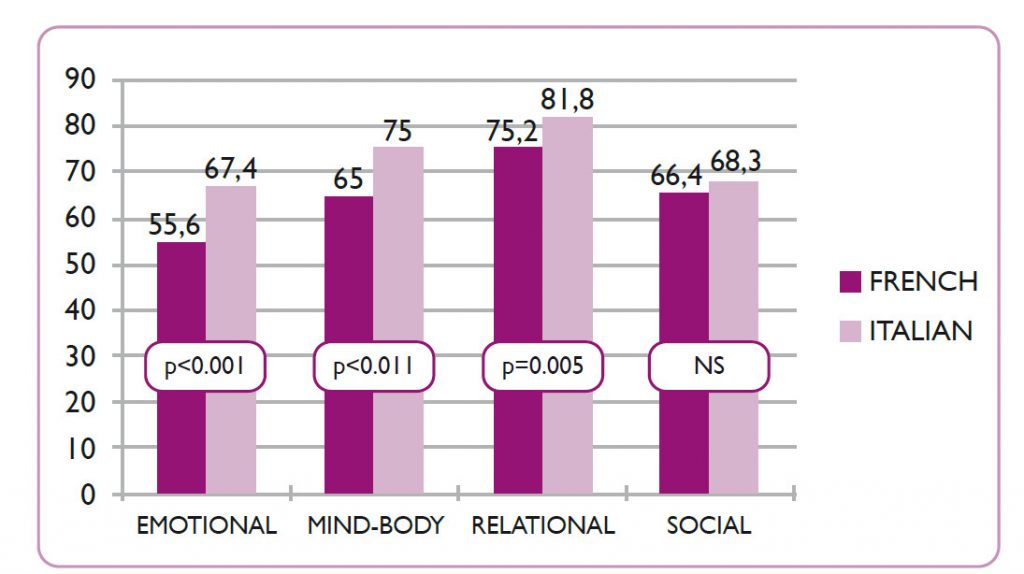
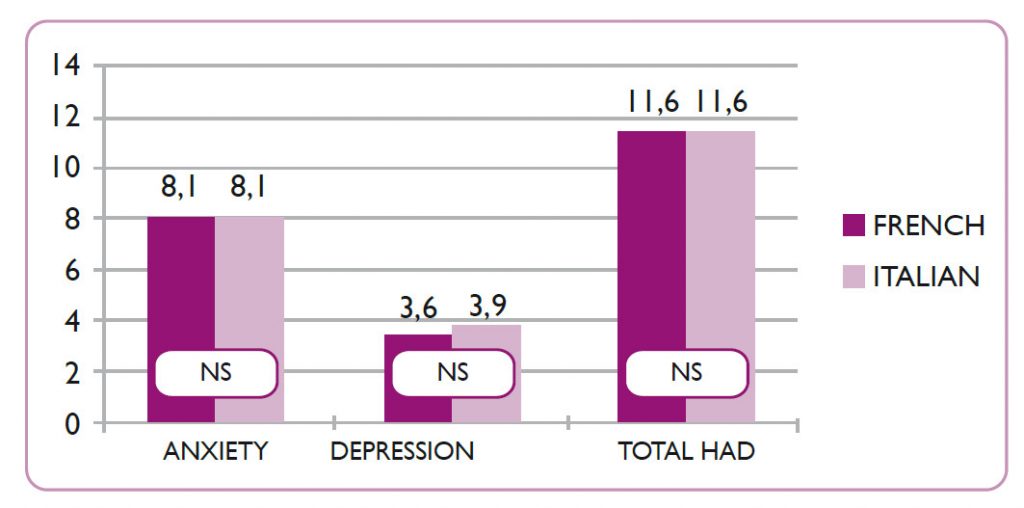
We are also committed to better understanding our patients’ emotional needs. In collaboration with the group of Dr. Sofia Gameiro at Cardiff University, in a study recently published in Human Reproduction we directly asked our patients the perceived usefulness of psychological services and measured their quality of life, anxiety, and depression levels through the validated tools FERTIQoL and HADS (Madero 2016). We have found some differences in the quality of life related to infertility of patients coming to Spain for IVF with donated oocytes depending on the country of origin (Figure 3). No differences in anxiety and depression symptoms were found (Figure 4).
At present, we are evaluating the context of family formation in single women, the psychological impact of replacing own gametes by donated ones, and the improvement of patients’ comfort with the development of more user-friendly treatments and protocols.
Patient-centered care (Fertility knowledge and awareness)
Fertility and reproduction are subject matters often surrounded by misconceptions, myths and knowledge gaps. Main aspects reflecting unawareness are: fecundity along the menstrual cycle, impact of unhealthy habits on reproduction, effect of toxins and pollutants on fertility, and age-related fertility decrease, especially in women.
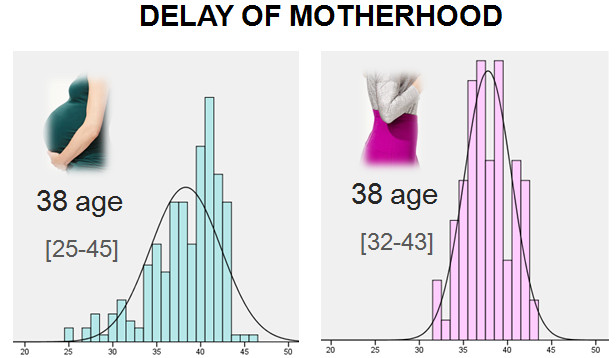
It is well established that female fertility decreases with age in a non-linear way. Female fertility is maximal between 20 and 25 years old and after starts to decrease, slightly in the late twenties and more markedly from 35 years onwards (Dunson et al., 2002, Dunson et al., 2004).
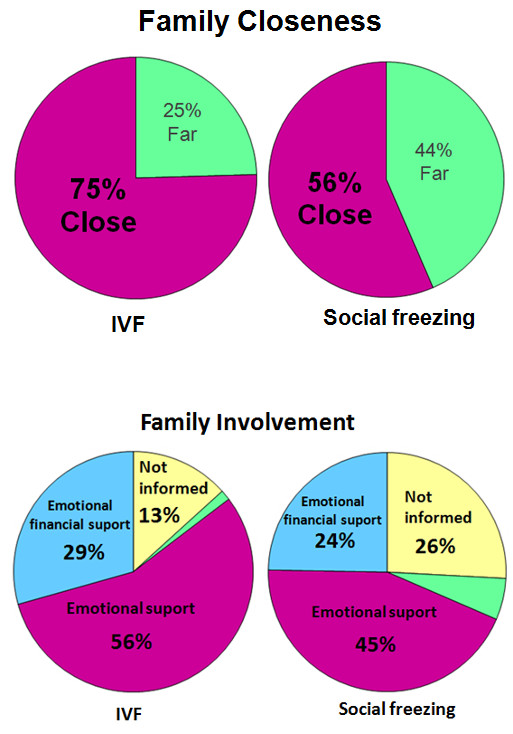
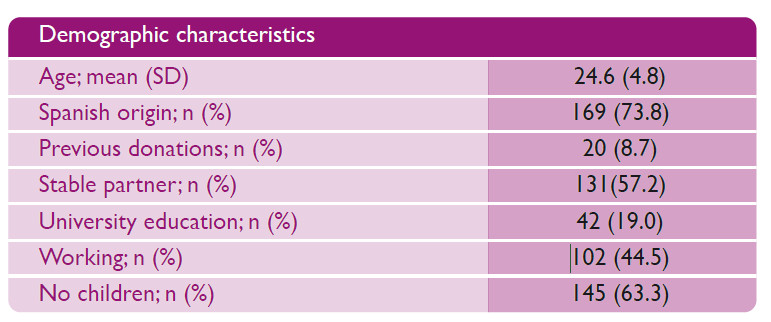
We are interested in studying how this knowledge is being translated into general people, including young women candidate to become oocyte donors in our center (Figure 7) (García et al. 2015, García et al. 2016), and physicians, including family doctors and gynecologists not specialized in ART (García et al. 2017).
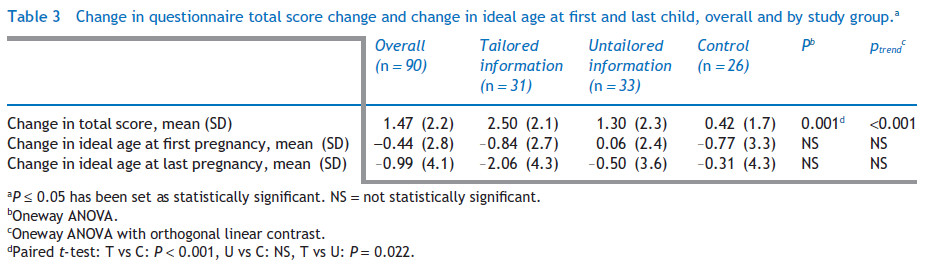
Ultimately, we are directing our efforts towards educational interventions as providing personalized information (García et al. 2017) (Figure 8) and organizing informative sessions aimed to increase fertility knowledge wherever necessary.
LABORATORY
Embryo development and selection (Project Leader: Meritxell Martínez)
The morphology and viability evaluation are important parameters for the success rate of IVF cycles. We are constantly testing techniques and procedures to select the best possible for embryo transfer. For this purpose, we use the well established embryo morphology classifications based on morphokinetic parameters. In our laboratory we use Time Lapse Systems (TLS) to evaluate embryo development using a proprietary algorithm that we are constantly improving. In addition, in collaboration with Dr. Josep Santaló of the UAB, we have used TLS to demonstrate that oocyte vitrification does not affect the timing of early developmental events of embryos derived from them (M. Martínez et al.2016). We have also validated the reliability of the TLS technique to determine early developmental milestones (M. Martinez, manuscript in preparation).
In vitro Maturation of MI (Noemí Martín)
Frequently, a portion of the oocytes is still immature at the time of oocyte pick-up. In ART patients, about 4% of all retrieved oocytes are at the immature non-GV stage. If these immature oocytes could be matured in vitro, the total number of mature oocytes obtained would increase and consequently a higher number of embryos would be obtained per cycle, possibly increasing the changes of pregnancy and live birth. Culture conditions are crucial for a correct maturation in vitro of immature oocytes. Nevertheless, there is scarce information available in the literature on either the most appropriate maturation protocol for immature oocytes, or the reproductive potential of embryo generated from in vitro matured MI oocytes. Because of this, we are currently evaluating two in vitro maturation media, in order to identify which of them provides better reproductive outcomes.